On January 10, a healthy 49-year-old man came down with headaches and blurry vision. He was participating in the test of an experimental drug that might help dull nerve pain, and it was the fifth day in a row that he’d taken the medicine.
The symptoms were serious enough to land the man in the hospital. Despite the fact that he was experiencing stroke-like symptoms, five other healthy volunteers received a sixth dose of the experimental medicine at the highest dose used in the study the next morning.
Two hours later, the hospital called Biotrial, the company running the study, to say that an MRI scan showed the hospitalized man had had a massive stroke in the brain stem. Later that day, he was declared brain dead. He died January 17, a week after checking into the hospital. According to French newspapers, he was Guillaume Molinet, an artist and father of four.
The five other volunteers who got the highest dose of the drug were then hospitalized. One was free of symptoms. But four had headaches, were fading in and out of consciousness and had short-term memory problems. Brain scans showed that they had identical, symmetrical brain injuries in two parts of the brain.
The study was the first one to try the drug in humans. Healthy volunteers were recruited to test preliminary doses for the drug and its safety in a so-called phase 1 study.
Independent Investigation Finds Missteps
The situation was totally unexpected, said Bernard Begaud, a pharmacologist at the University of Bordeaux in France. “The brain imaging was very strange, unlike anything we know in medicine,” he says.
He led the independent scientific investigation of what went wrong. Their report, released in April, outlined hypotheses on what happened and called for some changes in how clinical trials are conducted. The group concluded that the trial followed the rules and was perfectly legal but suffered from missteps.
None of the other 90 volunteers exposed to the drug at lower doses experienced any problems. “It was like a threshold,” said Begaud. There were no problems for people who had taken 20 milligrams of the drug for 10 days straight. But for those taking doses of 50 milligrams, the fifth day “was a disaster, suddenly,” he says. “It’s absolutely catastrophic, for medical research and of course for the volunteers.”
In a presentation to outside investigators, Biotrial called the reaction an “explosive and delayed toxicity not simply related to exposure levels.”
There were mistakes that came from ignoring common sense, Begaud said.
First, the people running the trial gave extremely high doses of the drug – about 40 times the amount that they expected was needed to quell pain. Their goal in the study was to completely block a certain enzyme. They’d increased the dose given to different subject groups in an odd pattern, too. Second, they ignored the fact that one participant was hospitalized and proceeded to give another high dose to five more people. Third, Begaud said, the trial was a “fishing expedition.” The drug hadn’t shown much promise for treating pain, but the company decided to test it in humans anyway.
Biotrial conducted the study in Rennes, France, for a Portuguese firm called Bial, developer of the experimental medicine.
The drugmaker defended its approach. “The dosage estimation over the trial was fully in accordance with the Protocol approved by the French authorities,” Bial representative Susana Vasconcelos told Shots in an email.
According to a Bial press release, the experimental drug, BIA 10-2474, was primarily meant to act “in the area of pain,” specifically to treat nerve pain, but also potentially chronic pain, anxiety and the tremors related to Parkinson’s disease.
A Search For New Way To Relieve Pain
The drug appears to work on the endocannabinoid system in the brain. That’s a collection of receptors in the brain and nervous system involved in pain and stress response (and also in getting high from smoking weed).
But in this case, the compound likely also acted on parts of the brain that didn’t have anything to do with endocannabinoid system, according to Daniele Piomelli, a pharmacologist at the University of California, Irvine. (He wasn’t on the scientific committee that investigated the trial).
Piomelli’s research group in California was involved early on in identifying this family of drugs, which has since gotten a lot of attention in the pharmaceutical world. He said the compounds were particularly attractive because they had the potential to do the beneficial things that smoking weed can do, like reduce anxiety and relieve pain, without serious side effects, such as memory loss.
Specifically, the compound prevents an enzyme called fatty acid amide hydrolase, or FAAH, from breaking down a molecule in the brain that’s involved in the body’s response to pain and anxiety. “The January tragedy was a surprise and a shock to everybody,” said Piomelli. “All the other FAAH inhibitors that had been tested in the past had been shown to be totally safe.” He says even mild side effects were rare. “What happened in Rennes didn’t match with anything we knew.”
The scientific committee investigating the trial hypothesizes that the bad effects likely resulted from the repeated high doses. They say the drug may have accumulated in the volunteers’ bodies enough to trigger an unexpected side effect.
Other drug companies had ditched similar molecules because they weren’t very effective. And BIA 10-2474 hadn’t shown much promise for pain relief.
“I still don’t understand why they would bother,” said Steve Alexander, a molecular pharmacologist at the University of Nottingham Medical School. “Most drug companies … would move on and go and look for something with a higher potency and a better selectivity.”
“As it is usual, at this early stage of evaluation in healthy volunteers no specific therapeutic target had been selected,” an email from Bial’s Vasconcelos said. “However, as described in the clinical trial protocol, it aimed to evaluate the potential effects of the compound on the endocannabinoid system, namely in pain sensitivity.”
Furthermore, the email said, “preclinical tests on animals performed with higher doses to the ones administered on the phase 1 clinical trial, did not show any evidence that could have prevented conducting the trial in man.”
Begaud and his colleagues recommend that clinical tests of a drug shouldn’t be started until there is a clear understanding of the benefits the work might give. “We feel that we have to change this paradigm — to first prove the potential and after we go to toxicology and if it’s safe we jump to humans,” Begaud said.
Of the four surviving volunteers who were hospitalized, two continue to have memory problems and other issues from their brain injuries, like vertigo and seeing double, he says. Many of the 90 volunteers exposed to the drug at lower doses are being monitored with brain imaging and neurological exams, and none have shown any problems.
Alexander says there may have been a hint from animal studies about potential problems. Two mice and a rat that died in toxicology studies showed brain damage, especially to the hippocampus, much like that of the affected volunteers. Such injuries happen a lot in drug studies on animals but not, Alexander said, with FAAH inhibitors.
“The fact that what they observed was an inflammatory response in the brain, which is entirely contrary to what one would expect from an FAAH inhibitor — that to me would have been, not a red light, but an amber light,” said Alexander.
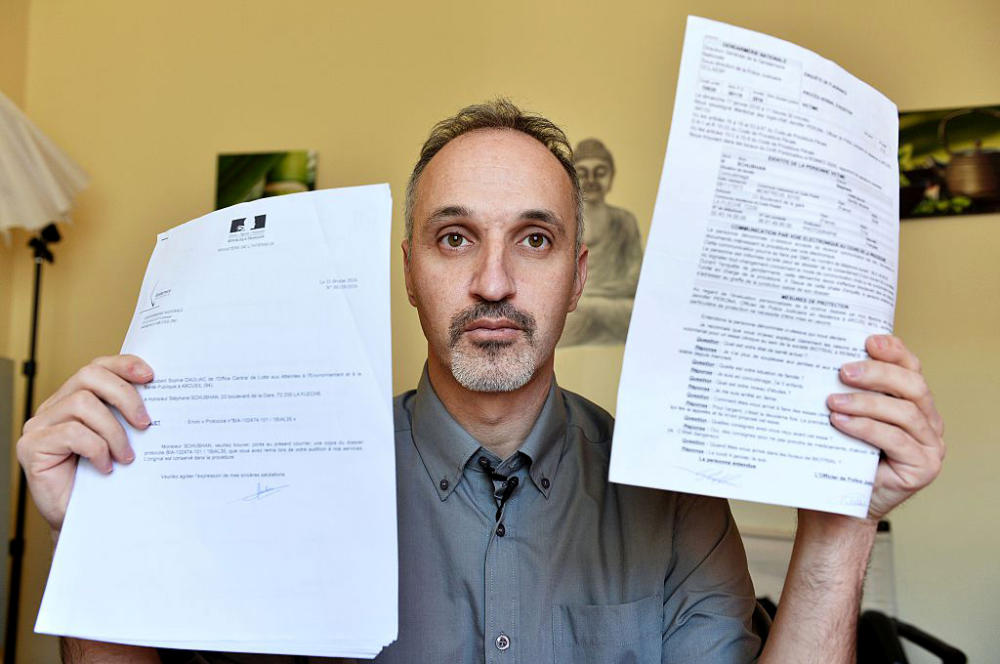
Stephane Schubhan, one of the men who was hospitalized and continues to have symptoms, told The Irish Times that he hadn’t heard about the animals dying in pre-clinical trials.
Other Studies Put On Hold
Properly informing volunteers about their risks is a challenge across the world, said Rebecca Dresser, a medical ethicist with Washington University in St. Louis. The first time a drug is tried in humans is the most dangerous period in drug development, but she says subjects often don’t understand the risks of participating.
“That requires conversation, back and forth. It’s like teaching, not just reciting a bunch of information to people,” said Dresser.
“Their trials were not badly designed,” says Piomelli, aside from the unusual dosing. “But at the end of day it’s not just following the rules. You need to have common sense.”
“If you have a patient in the hospital hospitalized with what looks like a stroke and you go ahead and do another set of administrations, quite frankly, I find this criminal, because this is an act of total lack of conscience,” says Piomelli.
He says the consequences from the failed trial could be huge for his field of research and for phase 1 trials.
After the news from France, Janssen Pharmaceuticals, a unit of Johnson & Johnson, halted research on similar compounds. And three Yale University trials using FAAH inhibitors were suspended until further notice. The Food and Drug Administration said it couldn’t comment on clinical holds unless they’re first disclosed by the company or institution sponsoring the research.
“The only silver lining, if there is one in this story, is that possibly in the future guidelines will be put in place to prevent this from happening again,” said Pomelli. But, he said, it’s a meager silver lining.
9(MDA3MTA1NDEyMDEyOTkyNTU3NzQ2ZGYwZg004))