One of the biggest challenges American hospitals face right now is moving to electronic medical records from old-fashioned paper files.
The switch is costing tens of billions of dollars, eating up tons of staff time, and it’s especially tough for the country’s 2,000 rural and small-town hospitals.
Rural hospitals are typically short on cash and people with information technology skills. So a lot of small hospitals are turning to bigger hospitals for help, and giving up some independence in exchange. The 10-bed Beartooth Billings Clinic in Red Lodge, Mont., is one hospital that did.
Red Lodge, a historic mining town just outside Yellowstone National Park, is about 60 miles west of Billings. On a recent spring day, the only thing slowing cars on Main Street in Red Lodge is a flock of wild turkeys strutting across the pavement.
Just days before, though, the road was covered with two feet of snow. Getting in and out of Red Lodge can be a real problem, as Dr. Billy Oley knows. He lives just a few miles from Beartooth Billings Clinic, at the hospital here.
“There was a time that the nurses won’t let me forget,” he says. “I drove my tractor to work one day because I couldn’t get my truck here. I had to plow with the tractor all the way to the hospital, and I just kept it here.”
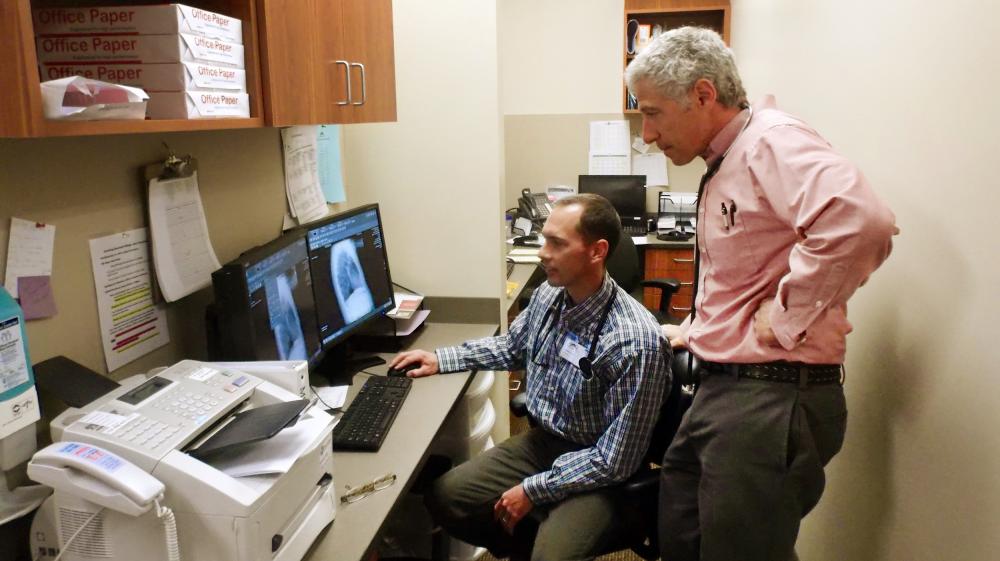
On days like that, Oley and his patients are particularly grateful for his hospital’s electronic medical records. He can share patient information instantly and securely with the big hospital in Billings and get expert advice whenever he needs it.
“We see a lot of patients who are able to not have to travel or see specialists, or do different things because we can just take care of it here,” Oley says.
Sharing electronic records sounds simple. But for a lot of little hospitals doing that while meeting new federal digital standards means coming up with $1 million or more up front. That’s a tall order, when the average rural hospital runs at a financial loss of 8 percent a year.
So the Red Lodge hospital became part of the bigger Billings Clinic system, in part to get help with IT. When hospitals align or merge, they give up some, or maybe all, control of their operations – everything from which records system they’ll use to which doctors and services are available where.
But affiliating with a big network often has benefits and can improve the care available in small towns.
Scott Duke with the Billings Clinic system says a lot of small hospitals are weighing trade-offs like Red Lodge’s in return for help for EMRs.
“To almost everyone we talk to, the EMR is right there” as a top concern, Duke says.
But for many rural hospitals it’s a point of pride, and matter of survival, to stay independent, and make their own decisions about the future.
A four-hour drive west from Red Lodge, the little town of Anaconda, Mont., sits in a fold of steep mountains and lush forests. The hospital there is a scrappy independent, and a proven survivor. It’s got 25 beds, and executive Meg Boynton says people in the area rely on it for everything from complex surgeries to routine care.
“We average about 36 to 50 births a year,” she says.
This building opened in 1981. The year before, a giant copper smelter shut down, leaving a lot of empty buildings in town. The economy remains marginal.
Steve McNeece, the hospital’s CEO, says it survives because they never get too comfortable. “Part of our goal and mission is to have a culture that embraces change and challenge,” he says.
McNeece’s hospital, unlike many in small towns, can find the $1.5 million it needs to finance the digital upgrade. He says it’s an obvious improvement over the old way they used to transfer patient information. “Put in a manilla folder and put it on the patient’s abdomen when they’re in the ambulance going to Saint Pat’s,” he laughs.
Anaconda’s hospital looks as though it’s going to be able to adopt the latest information technology and stay independent. But its fate is still tied to bigger hospitals in the area. It only makes sense for Anaconda to use the same records system as the places where the hospital refers patients for more specialized care.
“That was really the main driver in our decision-making. From a patient care perspective, this seemed like a safe and wise decision,” says McNeece.
Whether rural hospitals choose to do their digital upgrade independently, or partner with a bigger system, it’s important they have a conscious digital strategy, says Brock Slabach, a vice president with the National Rural Health Association.
“We’re very concerned about a digital divide that might be created going forward between the urban haves, if you will, and the rural have-nots,” he says.
Slabach worries hundreds of hospitals aren’t meeting new digital benchmarks as time to take advantage of federal help is running out. Starting this October, hospitals that don’t meet digital records standards will be hit with financial penalties, which would make the digital leap even harder to pull off.
This story is part of a partnership between NPR and Kaiser Health News.
9(MDA3MTA1NDEyMDEyOTkyNTU3NzQ2ZGYwZg004))